The Division of Developmental Disabilities has long identified the need for an integrated electronic Case & Financial Management System to standardize, centralize, and automate the service planning and billing process for individuals with an intellectual or developmental disability receiving Medicaid waiver and other State plan services.
The Division is seeking to procure and implement a new electronic Case & Financial Management System (ConneXion) to support the lifecycle of consumer care including information and referral; intake; assessment and reassessment; person centered care planning and service authorization; service delivery and payment; case closure; and reporting. Additionally, the Division's case management solution will support fraud, waste and abuse detection.
The Division is currently in the Planning & Procurement phase of the project. The Division anticipates a Request for Proposal (RFP) will be released for bid in late 2025.
- Project Objectives and Anticipated Benefits
The high-level objectives for the new case management solution are listed in the table below.
Project Objectives and Anticipated Benefits of Case Management Solution: - Improve efficiency and effectiveness of HCBS waiver programs that will lead to increased productivity and better customer service.
- Improve health outcomes for individuals with development disabilities through appropriate supports and services to enhance quality of life.
- Improve capability to prevent and reduce fraud, waste and abuse.
- Increase staff, client and provider satisfaction by providing on-line capabilities and automated processes.
- Improve access and services to clients through more consistent and efficient processes and automated workflows.
- Increased program transparency, accountability and reporting capabilities through more robust data collection/analytics and automated management tools.
- Facilitate compliance with CMS waiver requirements including specific quality improvement performance measures.
- Facilitate efficient data interchange and effective communication among waiver stakeholders and partners.
- The Division has summarized the key benefits from an enterprise case management solution:
- Provide online, real-time status of applications for DD services to individuals and their family/guardians and provide online, real-time status of contract enrollment applications to providers.
- Decrease processing time for ISP development and authorization,
- Decrease the percentage of Individual Support Plans (ISP) finalized after the implementation date,
- Improve ability to enforce rate methodology in ISPs finalized and service authorizations based on required assessments,
- Provide online, real-time information for staff, providers and individuals/families on ISPs and services delivered,
- Eliminate the need to route paper documentation to support case management processes,
- Provide online, real-time dashboards and/or reports for supervisors, managers and Quality Assurance staff,
Reduce time needed to track and report quality improvement measures and increase accuracy of quality performance measures.
- Benefits for Division Providers:
- Service Providers
- Ability to view the profile, demographics and service plan and know the status of the plan in real time,
- Access to use internal messaging center to be able to connect more efficiently with individuals and other team members,
- Submit and mange claims (similar to current functionality in CIMOR),
- Access to online reports to use for financial planning,
- Ability to do your own voids/rebills, if desired,
- Access to complete consumer referral and mortality review as they will be moved to ConneXion, reducing the number of applications a provider has to log into,
- Ability to review individual benefit data in the system.
- Targeted Case Management (TCM) Providers
- ConneXion will be a single source of information for an individual's profile, demographics and service plan with the ability to know the status of the plan in real time,
- Access to use internal messaging to be able to connect more efficiently with individuals/families and other team members,
- Ability to utilize tasks lists, reminders and work lists to drive workflow efficiencies,
- Single source of case notes for an individual, the handoff of care to other entities will be more efficient since it is a single record for the individual,
- Access to reports to use for support and financial planning,
- Support monitoring will be encompassed with plan development in ConneXion system.
- Service Providers
- Project Team
- Meet the Division’s ConneXion Executive Leadership & Project Management Team:
- HealthTech Solutions (HTS) was awarded the Planning & Procurement Vendor Support contract for the ConneXion project in May 2024.
Project Owner Interest or Role Val Huhn DMH Executive Sponsor Cynthia Hassler ITSD Executive Sponsor Team Member Interest or Role TBD DMH Project Sponsor Angie Brenner DMH Business Sponsor Wendy Witcig DMH Business Sponsor Molly Boeckmann DMH Director of Administration Richard Kliethermes DMH IT Director Liaison Jamie Bish DMH Project Director Jennifer Harrison DMH Project Manager Samridha Rana DMH Project Coordinator Shannon Hoerschgen DMH Configuration Architect Adil Khan DMH Solution Architect Gary Schanzmeyer DMH Billing/Claims Specialist Rick Shuey DMH Systems & Data Specialist Cynthia McGee ITSD PM Oversight Shaun Settle ITSD Project Manager - Meet the Division’s ConneXion Executive Leadership & Project Management Team:
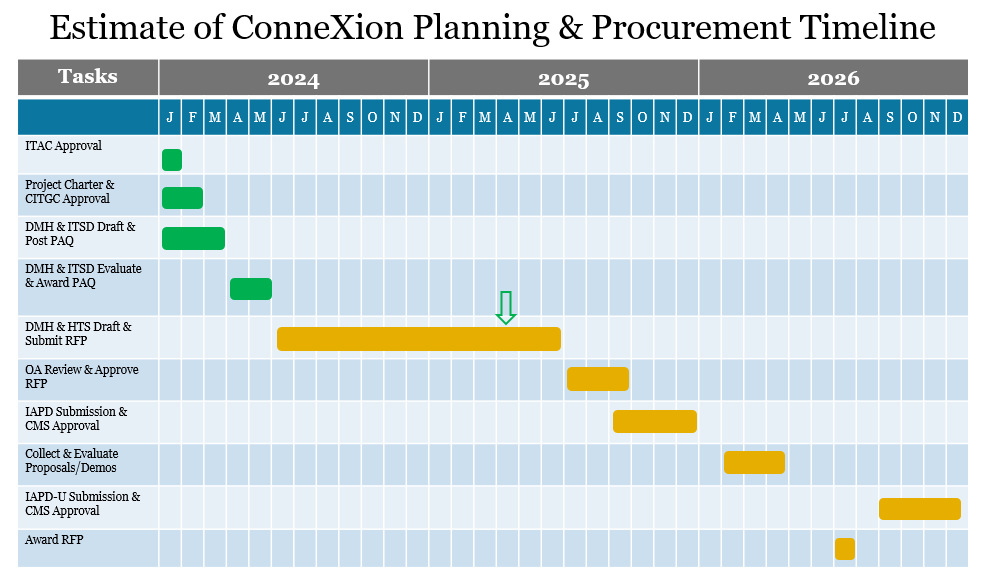
- Project Timeline
Estimated ConneXion Timeline:
- Overall Project Timeframe: February 2024 - June 2034
- Planning & Procurement: February 2024 - December 2026
- Phased Implementation: December 2026 - September 2030
- Operation & Maintenance: September 2030 - June 2034
- Overall Project Timeframe: February 2024 - June 2034
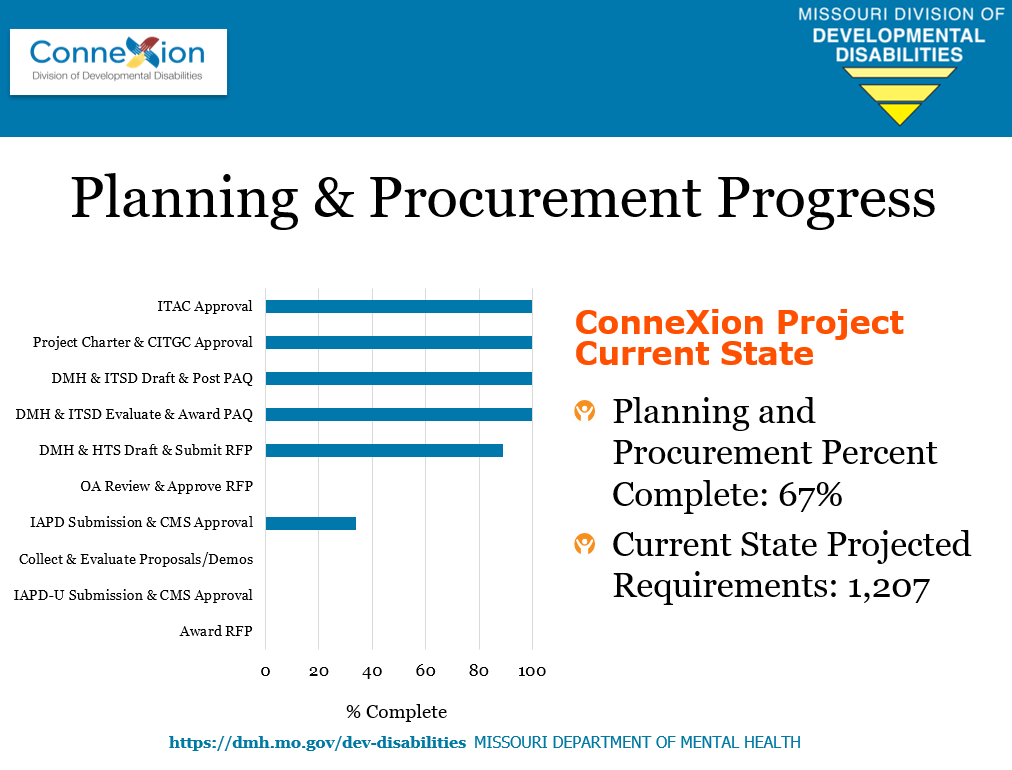
- Planning and Procurement Progress
*Progress Update on 4/15/2025
- Scope
The ConneXion - DD Case & Financial Management System will support comprehensive case management from the initial inquiry for services to case closure, including information and referral, intake, assessment and reassessment, person centered care planning and service authorization, provider enrollment and management, service delivery and payment, case closure, quality assurance, and reporting.
End-users of the ConneXion system will include DMH and Division of DD staff, Service providers, and Targeted Case Management (TCM) providers. Individuals/families/guardians will have limited access to the system via the person portal.
- The scope of the project does include:
- The case management system will be utilized for the Division's HCBS waiver and additional state plan programs including Case Management Only, Resource & Referral, Choices for Families, Autism and other non-waiver programs.
- The scope of the project does not include:
- Applications supporting internal operations for the Division's State Operated Programs (SOP) at habilitation centers, Northwest Community Services and Southwest Community Services.
- Full CIMOR Replacement, this is not a complete CIMOR replacement project. The following functions will still be conducted in CIMOR as listed below:
- EMT (Event Management Tracking);
- Consumer Banking functions;
- Pay and Chase claim adjudication;
- Room and Board services;
- SAMII (MOVERS) interface for non-Medicaid services; and
- Provider administrative payments (shared unit).
- Electronic Visit Verification will not be a module implemented in this system.
- The scope of the project does include:
- Communication and Resources
Please see below for resources & education pertaining to the ConneXion project including communications, presentations, and other applicable resources.
ConneXion Planning and Procurement Kick Off Meeting